ORIGINAL ARTICLE | https://doi.org/10.5005/jp-journals-10002-1302 |
Central Compartment Nodal Disease in Small Papillary Thyroid Carcinomas in Singapore
1,2Department of General Surgery, Changi General Hospital, Singapore
Corresponding Author: Nern H Kao, Department of General Surgery, Changi General Hospital, Singapore, Phone: +65 6850 3551, e-mail: kao.nern.hoong@singhealth.com.sg
How to cite this article Kao NH, Koh AJH. Central Compartment Nodal Disease in Small PTCs in Singapore. World J Endoc Surg 2020;12(3):109–112.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Background: Prophylactic central compartment clearance has been a debate for early papillary thyroid carcinoma (PTC). The American Thyroid Association recommends total thyroidectomy alone for small tumors without clinical nodes. However, we note a high incidence of nodal disease within our practice. This study aims to evaluate the incidence of metastatic central compartment nodes in small (%3C;4 cm) PTC. Secondary aims included postoperative hypoparathyroidism and recurrent laryngeal nerve injury.
Materials and methods: A retrospective cohort study was performed evaluating patients who had thyroid surgery from January 2011 to October 2016. Patients with total thyroidectomy alone were compared with those with prophylactic central neck dissection (pCND). Histology was reviewed for tumor size and nodal disease.
Results: One hundred and six patients were recruited for this study. More than half of thyroidectomies with pCND were found to be positive (36/57). This is regardless of tumor size, although tumor %3E;20 mm was more likely to have a nodal disease (OR 2.40 95%; CI 0.58–9.87; p = 0.23). T3 disease was more likely to have a nodal disease (15/21 sides) (OR 1.79; 95% CI 0.56–5.67; p = 0.33). More patients in the pCND arm developed transient hypoparathyroidism (14/22 vs 4/17) but all resolved within a year. One patient developed hoarseness alone while three patients reported dysphagia in the pCND arm compared to one patient in the total thyroidectomy arm with dysphagia.
Conclusion: More than half of patients with PTC (<4 cm) have metastatic central compartment nodes. Prophylactic central neck dissection can be safely performed. However, we still lack adequate data on long-term effects.
Keywords: Central compartment, Lymph nodes, Metastases, Micropapillary, Papillary thyroid, Thyroid cancer.
INTRODUCTION
Thyroid cancer is the most common endocrine malignancy and the eighth-most common cancer in Singaporean female. Recent local epidemiology studies have shown a rise in the age-standardized incidence rate to approximately 9.5/100,000.1 Another local study by Shulin et al. showed that the incidence of papillary thyroid microcarcinoma has risen by 80% over the last few years. Shulin et al. also showed that the incidence of papillary thyroid carcinoma (PTC) larger than 5 cm was only 5%.2 This suggests that patients are presenting earlier with small volume thyroid cancers and therefore undergo surgery early.
According to the American Thyroid Association (ATA), thyroidectomy alone without central compartment neck dissection is sufficient for small (<4 cm) non-invasive PTCs.3 However, the presence of central compartment nodal metastases is a known predictor of poor overall survival outcome and locoregional recurrence.4–6 Numerous studies have shown that prophylactic central neck dissection (pCND) helps to decrease the locoregional recurrence rate. A recent meta-analysis performed by Zhao et al. of 20 studies showed the overall recurrence rate to be significantly lower when pCND was performed in combination with a total thyroidectomy compared to a total thyroidectomy alone (5.9 vs 7.2%) for PTC. The presence and characteristics of the lymph node metastases also help to identify patients that will require radioactive iodine (RAI) therapy as well as the dose required.7–9
Within our clinical practice, we have observed several patients with central compartment metastases even with a small tumor size. This study aims to evaluate the incidence of central compartment nodal metastases within our local population to guide our future decisions for pCND for small tumors (<4 cm). The primary objective will be to assess the incidence of central compartment lymph nodes in small PTC. The secondary objectives include postoperative hypoparathyroidism and recurrent laryngeal nerve (RLN) injury rates.
MATERIALS AND METHODS
Data were collected from our patients from a single institution over 5 years from January 2011 to October 2016. All patients who had undergone either a hemithyroidectomy (primary or completion) or a total thyroidectomy within our center were included. Surgery was performed either by a senior consultant or by a resident under supervision. Patients were excluded if they had had previous ipsilateral neck surgery or radiotherapy to the neck. Patients who did not have postoperative histological confirmation of PTC or who had a tumor size of >4 cm were also excluded. All data were collected retrospectively through a review of both electronic records and outpatient clinic notes. Histology reports of identified patients were reviewed for the presence of central compartment lymph nodes.
Postoperative hypoparathyroidism was evaluated with serial serum intact parathyroid hormone levels (iPTH) before discharge and at follow-up. Hypoparathyroidism was defined as iPTH ≤1 pmol/L. Patients were usually treated with oral calcitriol and calcium replacements if found to be hypoparathyroid. Patients received intravenous calcium replacement if they were symptomatic or severely hypocalcemic (corrected calcium levels ≤1.9 mmol/L).
Patients with RLN injury were assessed subjectively according to the patient’s perception of hoarseness or dysphagia. Both inpatient and outpatient notes were reviewed for these complaints as well as the need for fluid thickeners or nasogastric tube (NGT) feeding. Patients did not routinely undergo nasoendoscopic evaluation of the vocal cords unless they complained of significant persistent hoarseness or dysphagia at follow-up.
RESULTS
Study Characteristics
A total of 122 patients had undergone thyroid surgery within our center during the accrual period. Of these, 16 patients were excluded as postoperative histology was either benign, tumor size of >4 cm or showed follicular cancer. As such, 106 patients were recruited for the study with a total of 108 thyroidectomies (2 patients underwent completion thyroidectomy during the accrual period).
The mean age of our patients was 52 years (19–101 years) with the majority being female (74%) and above 45 years of age (73%). The Chinese ethnicity was predominant (67.9%) within our study population (Table 1).
Thyroid surgery is usually performed via an open lateral approach in our center. However, five of the patients underwent endoscopic surgery. These five patients all had thyroidectomy alone without CND.
Central Compartment Nodal Disease
Postoperative histology was reviewed for all recruited patients. Patients who had undergone total thyroidectomy with bilateral CND had each side evaluated separately for nodal disease for the study. This gave us a total of 57 sides from 54 patients. More than half of the patients who had undergone CND were found to have a nodal disease (36/57 sides). Patients with T3 disease (tumor extension beyond the thyroid) were more likely to have a nodal disease (15/21 sides) (OR 1.79; 95% CI 0.56–5.67; p = 0.33). Sub analyses according to tumor size was also performed to help identify future patients preoperatively who may benefit from pCND. This showed that more than half the patients had nodal disease regardless of the size (Figs 1 and 2). This trend was even more prevalent the larger the tumor size. Patients were more likely to have a nodal disease with tumor size >20 mm (OR 2.40; 95% CI 0.58–9.87; p = 0.23).
Hypoparathyroidism
Patients who had undergone a completion thyroidectomy or a total thyroidectomy were included in the analysis for hypoparathyroidism (Fig. 3). Twenty-one patients were excluded as they either had concurrent surgery for hyperparathyroidism or did not have serial serum iPTH. None of the patients who had a completion thyroidectomy developed hypoparathyroidism. These patients also did not receive CND. 4/17 patients in the total thyroidectomy alone arm developed hypoparathyroidism while 14/22 patients with pCND had hypoparathyroidism. Of these 18 patients, 11 (2 vs 9) were still hypoparathyroid at discharge. Seven (2 vs 5) patients still had low iPTH levels at their first follow-up but all had resolved by the first year (Fig. 4). Patients with CND were more likely to develop hypoparathyroidism than those who did not (OR 2.70; 95% CI 0.75–9.72; p = 0.13).
Recurrent Laryngeal Nerve Injury
Significant RLN injury rates were low in our study population. None of the patients who had undergone a hemithyroidectomy regardless of CND developed significant symptoms. 1/26 patients in the total thyroidectomy arm had dysphagia requiring NGT feeding. This patient had undergone an emergency total thyroidectomy for airway compression from the goiter. Patients who had received CND had an expected higher rate of symptoms. Of the 51 patients, 1 patient had hoarseness alone while another 3 complained of dysphagia as well. Only one required NGT feeding. None of the symptomatic patients was from the bilateral CND arm. However, one patient from the bilateral CND arm was excluded due to dysphagia from a dense perioperative stroke.
| Age, years | 52 (19–101) | |
|---|---|---|
| Gender | ||
| Male | <45 years | 7 |
| ≥45 years | 20 | |
| Female | <45 years | 21 |
| ≥45 years | 58 | |
| ASA status | ||
| I | 10 | |
| II | 62 | |
| III | 30 | |
| IV | 4 | |
| Race | ||
| Chinese | 72 | |
| Malay | 21 | |
| Indian | 1 | |
| Other | 12 | |
| Indication for thyroidectomy | ||
| Goiter | 40 | |
| Thyroid cancer | 65 | |
| Graves’ disease | 3 | |
| Hemithyroidectomy (n = 27) | ||
| T1a | 25 | |
| T1b | 0 | |
| T2 | 1 | |
| T3 | 1 | |
| Hemithyroidectomy with clearance (n = 2) | ||
| T1a | 2 | |
| T1b | 0 | |
| T2 | 0 | |
| T3 | 0 | |
| Total thyroidectomy (n = 27) | ||
| T1a | 22 | |
| T1b | 3 | |
| T2 | 0 | |
| T3 | 2 | |
| Total thyroidectomy with clearance (n = 52) | ||
| T1a | 9 | |
| T1b | 13 | |
| T2 | 9 | |
| T3 | 21 | |

Fig. 1: Incidence of nodal disease by tumor stage

Fig. 2: Incidence of nodal disease by tumor size
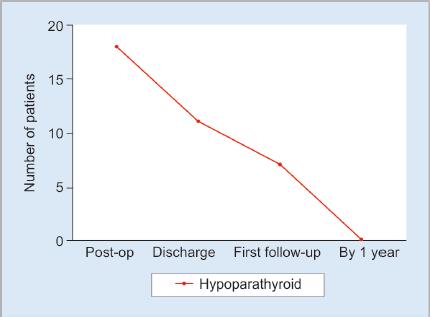
Fig. 3: Incidence of hypoparathyroidism

Fig. 4: Incidence of hypoparathyroidism post-total thyroidectomy
DISCUSSION
Our study shows that pCND can upstage more than half of the patients from N0 to N1a. This affects the patients by increasing the recurrence risk from low to intermediate. Treatment will also differ in that these patients will require RAI as well as a higher dosage required. The complication rates are comparable with other centers as there were no patients with permanent hypoparathyroidism and only one patient with persistent RLN injury.
Despite the numerous studies available, the role of pCND is still a matter of debate. The ATA recommends thyroidectomy alone without CND in small, non-invasive, clinical N0 tumors. This is because of studies that show that there is no improvement in the long-term patient outcome while exposing the patient to complications.10,11 Conversely, a meta-analysis of 23 studies by Chen et al. looking at pCND for PTC shows a significantly lower locoregional rate recurrence (LRR) (OR 0.65; 95% CI 0.48–0.88; p = 0.006). However, it is important to note that patients who receive pCND and are found to have the nodal disease will also receive RAI treatment. Radioactive iodine treatment has been shown to decrease the LRR and will therefore influence the overall survival.12 This suggests that the difference between patients with total thyroidectomy alone vs with pCND may be more significant than expected as patients with total thyroidectomy alone will have lost a further two modalities of treatment, i.e., lymphatic clearance and RAI treatment. Locoregional rate recurrence would necessitate reoperation and this exposes the patient to an increased risk of permanent RLN (0–5.8%) and hypocalcemia (0–9%) as per a meta-analysis by Shorook et al.13
LIMITATIONS
The main limitation of our study is the small study population. As such, we were unable to obtain any statistically significant results. Within this limitation, we can observe a similar trend found in larger studies.
The incidence of RLN neuropraxia may be higher than documented. There was no objective assessment for vocal cord palsy. Mild hoarseness may not have been adequately documented in the clinical notes. However, significant nerve injury would have also presented as dysphagia. Inpatient and outpatient notes were reviewed for symptoms, the need for fluid thickeners or NGT feeding to increase the pick-up rate.
Our patients are routinely given a follow-up within the first month followed by several follow-ups within the first year pending the need for adjuvant treatment and adequacy of thyroid suppression. Once these are adequate, patients are usually given annual follow-ups to monitor their thyroid suppression as well as the thyroglobulin (Tg) and thyroglobulin antibody (TgAb) levels. The mean follow-up duration was 37 months (1–85). This is not an adequate period to assess for disease-free survival (DFS) as PTC is known to be indolent and may take years before recurrence. This study is therefore not adequate to evaluate the long-term outcome benefits of pCND.
SUMMARY
The study shows that the incidence of central compartment nodal disease in small PTC is not low. We acknowledge that although it was not statistically significant, more than half of our patients were found to have nodal metastases following pCND. A thorough discussion should still be had with the patient concerning treatment choice, as the complication rates for pCND are acceptable.
REFERENCES
1. National Registry of Diseases Office. Singapore Cancer Registry.Annual Registry Report 2015.
2. Shulin JH, Aizhen J, Kuo SM, et al. Rising incidence of thyroid cancer in Singapore not solely due to micropapillary subtype. Ann R Coll Surg Engl 2018;100(4):295–300. DOI: 10.1308/rcsann.2018.0004.
3. Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016;26(1):1–133. DOI: 10.1089/thy.2015.0020.
4. Podnos YD, Smith D, Wagman LD, et al. The implication of lymph node metastasis on survival in patients with well-differentiated thyroid cancer. Am Surg 2005;71(9):731–734. DOI: 10.1177/000313480507100907.
5. Zaydfudim V, Feurer ID, Griffin MR, et al. The impact of lymph node involvement on survival in patients with papillary and follicular thyroid carcinoma. Surgery 2008;144(6):1070–1077. DOI: 10.1016/j.surg.2008.08.034.
6. Adam MA, Pura J, Goffredo P, et al. Presence and number of lymph node metastases are associated with compromised survival for patients younger than age 45 years with papillary thyroid cancer. J Clin Oncol 2015;33(21):2370–2375. DOI: 10.1200/JCO.2014.59.8391.
7. Zhao WJ, Luo H, Zhou YM, et al. Evaluating the effectiveness of prophylactic central neck dissection with total thyroidectomy for cN0 papillary thyroid carcinoma: an updated meta-analysis. Eur J Surg Oncol 2017;43(11):1989–2000. DOI: 10.1016/j.ejso.2017.07.008.
8. Barczynski M, Konturek A, Stopa M, et al. Prophylactic central neck dissection for papillary thyroid cancer. Br J Surg 2013;100(3):410–418. DOI: 10.1002/bjs.8985.
9. Ito Y, Miyauchi A, Masuoka H, et al. Excellent prognosis of central lymph node recurrence-free survival for cN0M0 papillary thyroid carcinoma patients who underwent routine prophylactic central node dissection. World J Surg 2018;42(8):2462–2468. DOI: 10.1007/s00268-018-4497-x.
10. Chisholm EJ, Kulinskaya E, Tolley NS. Systematic review and meta-analysis of the adverse effects of thyroidectomy combined with central neck dissection as compared with thyroidectomy alone. Laryngoscope 2009;119(6):1135–1139. DOI: 10.1002/lary.20236.
11. Viola D, Materazzi G, Valerio L, et al. Prophylactic central compartment lymph node dissection in papillary thyroid carcinoma: clinical implications derived from the first prospective randomized controlled single institution study. J Clin Endocrinol Metab 2015;100(4):1316–1324. DOI: 10.1210/jc.2014-3825.
12. Ruel E, Thomas S, Dinan M, et al. Adjuvant radioactive iodine therapy is associated with improved survival for patients with intermediate risk papillary thyroid cancer. J Clin Endocrinol Metab 2015;100(4):1529–1536. DOI: 10.1210/jc.2014-4332.
13. Na’ara S, Amit M, Fridman E, et al. Contemporary management of recurrent nodal disease in differentiated thyroid carcinoma. Rambam Maimonides Med J 2016;7(1):e0006. DOI: 10.5041/RMMJ.10233.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.