CASE REPORT |
https://doi.org/10.5005/jp-journals-10002-1430 |
Traumatic Hemorrhage of Adrenal Myelolipoma: A Rare Clinical Presentation
1-4Department of Surgery, Government Medical College & Hospital, Chandigarh, India
5Department of Radiodiagnosis, Government Medical College & Hospital, Chandigarh, India
Corresponding Author: Shivani Goyal, Department of Surgery, Government Medical College & Hospital, Chandigarh, India, Phone: +91 9888939785, e-mail: shivaniigoyal@gmail.com
Received on: 02 November 2022; Accepted on: 30 January 2023; Published on: 15 April 2023
ABSTRACT
Introduction: Adrenal myelolipomas are a rare benign tumor composed of mature adipose tissue and hematopoietic elements. The majority of cases are asymptomatic, most of them are diagnosed incidentally or as a result of developing complications due to the tumor.
Case description: This report presents an unusual case of a 34-year male who suffered pain abdomen after colliding with a motorbike. Abdominal examination revealed distension in right hypochondrium. CECT abdomen confirmed the presence of right adrenal myelolipoma with possibility of hemorrhage. Hence, the patient was successfully managed with right adrenalectomy.
Conclusion: After the initial diagnosis, management of myelolipoma should be done on case-to-case basis. Patients should be made aware of the various complications that could develop in future in case conservative management is chosen.
How to cite this article: Goyal S, Upadhyay R, Radhakrishnan R, et al. Traumatic Hemorrhage of Adrenal Myelolipoma: A Rare Clinical Presentation. World J Endoc Surg 2022;14(2):55-57.
Source of support: Nil
Conflict of interest: None
Patient consent statement: The author(s) have obtained written informed consent from the patient for publication of the case report details and related images.
Keywords: Bleeding, Incidentaloma, Myelolipoma.
INTRODUCTION
Myelolipomas of the adrenal gland are rare tumors. They are more commonly detected as incidentalomas because of the widespread use of radiological investigations. A large number of them are asymptomatic; symptoms arise either because of the large size of the tumor, or any associated complications (rupture and hemorrhage). Here we report a case where the adrenal myelolipoma was detected after the patient sustained blunt trauma abdomen.
CASE DESCRIPTION
A 34-year-old male presented to surgery emergency with a complaint of a fall over his abdomen after colliding with a motorcycle while he was walking. Postfall, he complained of dull aching pain in the right side of the abdomen. There were no other significant complaints in the form of loss of consciousness, respiratory distress, and nausea vomiting. There was no other significant past history. On palpation of the abdomen, there was abdominal distension occupying the right hypochondrium and extending into the epigastrium, right lumbar, and umbilical region. After subjecting the patient to a primary survey and finding him stable enough for radiological investigations, ultrasonography abdomen was done, which showed a large mass measuring 19 × 20 cm in the right retroperitoneum. Organ of origin could not be made out.
An abdominopelvic computed tomography (CT) scan (Figs 1 and 2) revealed a well-defined heterogenous mass measuring 19.6 × 20.4 × 15.1 cm arising from the right suprarenal region with nonseparate visualization from the right adrenal gland. The mass showed predominantly fat attenuation with nonenhancing soft tissue areas within. These findings were suggestive of right adrenal myelolipoma with the possibility of hemorrhage. This mass was closely abutting the inferior surface of the liver, ascending colon, hepatic flexure, duodenum, and inferior vena cava but with maintained fat planes. Laboratory tests, baseline blood investigations, serum cortisol, serum aldosterone, and urinary metanephrines were within the normal range.

Fig. 1: Abdominal CT scan showing a large well-defined right adrenal gland mass with fat attenuation

Fig. 2: Abdominal CT scan showing a relation of the mass to the liver and right colon
The patient was taken up for exploratory laparotomy through a right subcoastal incision. Intraoperatively a large mass was identified in the right retroperitoneum, which was displacing the liver upwards, hepatic flexure, transverse colon inferiorly, and duodenopancreatic complex to the left (Fig. 3). Surgery was proceeded by mobilizing the duodenum and right colon by a Kocher and Cattell-Braasch maneuver. The peritoneal attachment between the liver and mass was cauterized. The tumor was dissected free from the upper pole of the right kidney by a harmonic scalpel. Since the tumor was replacing the whole right adrenal gland, a transperitoneal right adrenalectomy was performed, and the specimen was sent for histopathological evaluation (HPE) (Fig. 4).
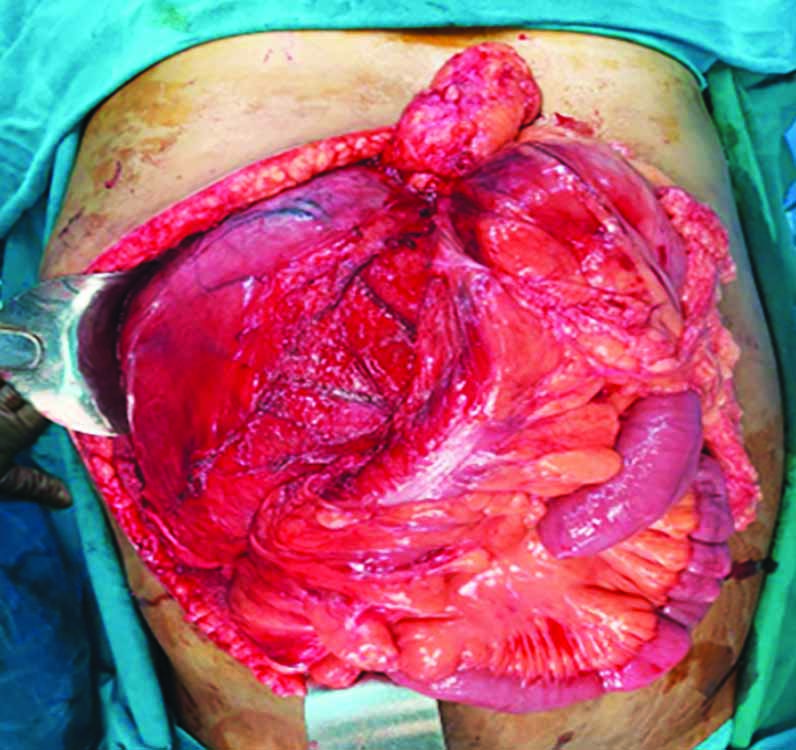
Fig. 3: Intraoperative image of the mass with the displacement of the right colon medially

Fig. 4: Image showing the encapsulated tumor
A gross examination of the specimen showed a large, rounded encapsulated mass with a smooth external surface with a size of 19 × 13.5 × 12.5 cm. The cut surface showed a grayish-yellow to a grayish-brown tumor (Fig. 5). Microscopy revealed a well-circumscribed tumor composed of mature adipose tissue admixed with hematopoietic elements consisting of erythroid, myeloid, and megakaryocytic lines, thus confirming the diagnosis of myelolipoma (Fig. 6).

Fig. 5: Cut surface of the tumor showing gray-brown to gray-yellow area

Fig. 6: HPE image showing adipocytes with hematopoietic element
DISCUSSION
The adrenal lipomatous tumor is defined as a group of adrenal tumors with a significant proportion of adipose tissue. Myelolipoma is the most common among them.1 They are rare, benign tumors. Adrenal glands are the most common site affected, but they can also be found in the pelvic region, thorax, mediastinum, and paravertebral region.2 Earlier, these lesions were detected only at autopsy, but with increasing use of various imaging modalities, the incidence has increased and range from 0.08 to 0.4%.3
The first case was reported in 1905 by Gierke, a German pathologist. The term adrenal myelolipoma was coined by Charles Oberley.4 World Health Organization in 2019 classified tumors of endocrine origin where adrenal myelolipoma is classified as a mesenchymal and stromal tumor of the adrenal cortex.5 Multiple theories have been proposed regarding the etiology of myelolipoma, such as the development from embryonic bone marrow remains, metaplasia cortical cells, embolism of bone marrow cells, or differentiation of previously uncommitted mesenchymal cells, but none is established.6
Adrenal myelolipoma are largely asymptomatic tumors. Clinically they are mostly inert.
Symptoms occur mostly due to reasons:
-
A hormonally active tumor (Cushing’s disease, Conn’s disease, Addison’s disease, and pheochromocytoma).
-
The large size of the tumor causing local compressive symptoms in the form of abdominal pain, nausea, and vomiting.
-
Complications of the tumor in the form of retroperitoneal rupture and hemorrhage within the tumor.7
In the case report mentioned above, the patient was completely asymptomatic before sustaining trauma. It is rather less likely for the patient to be completely asymptomatic, having such a huge myelolipoma. A plausible explanation could be that the patient may be harboring a small asymptomatic myelolipoma before trauma which expanded in size after the injury because of traumatic intratumoral bleed, making the patient symptomatic. Albala et al. have published a similar case report where trauma leads to hemorrhage within the myelolipoma, and the patient was treated with radical resection of the mass and kidney.8
The various differentials of a suprarenal mass with the fatty component are myelolipoma, renal angiomyolipoma, retroperitoneal lipoma, retroperitoneal liposarcoma, adrenal adenoma, or adrenocortical carcinoma.9 Diagnosis relies upon radiological examination. Ultrasonography is insufficient to make a diagnosis. Demonstration of fat density within an adrenal mass on CT scan is characteristic of myelolipoma lesion.6 The cut surface of tumor shows yellow color corresponding to the adipose tissue, while red to brown color corresponds to the hematopoietic tissue. Microscopic appearance has two constant features—dense adipose tissue and trilineage hematopoietic tissue (erythroid, lymphoid, and megakaryocytic).10
Formal management guidelines are lacking; the decision is made from case to case basis. No treatment is required in tumors which are asymptomatic and smaller than 5 cm in maximum size. Only routine follow-up is suggested in such cases.2 Surgical resection is indicated if the tumor is functional, increasing in size, becoming functional, or doubt of malignancy is present.11
Adrenalectomy is the surgery of choice which can be accomplished either via an open approach or laparoscopic approach in case of smaller lesions. In the case of bilateral myelolipoma, the larger one is removed and the patient is kept on routine follow-up for the other to prevent adrenal insufficiency.
CONCLUSION
While adrenal myelolipoma is rare, trauma leading to an increase in size (because of intratumoral bleeding) is even rarer. Such a possibility should be kept in mind while keeping these patients on conservative management and a similar should also be conveyed to the patient.
REFERENCES
1. Lam AK. Lipomatous tumours in adrenal gland: WHO updates and clinical implications. Endocr Relat Cancer 2017;24(3):R65–R79. DOI: 10.1530/ERC-16-0564
2. Heylen S, Hubens G, Vaneerdeweg W, et al. Giant adrenal myelolipoma: a case report. Acta Chir Belg 2011;111(2):91–93. DOI: 10.1080/00015458.2011.11680714
3. Settakorn J, Sirivanichai C, Rangdaeng S, et al. Fine-needle aspiration cytology of adrenal myelolipoma: case report and review of the literature. Diagn Cytopathol 1999;21(6):409–412. DOI: 10.1002/(sici)1097-0339(199912)21:6<409::aid-dc9>3.0.co;2-a
4. Ersoy E, Ozdogan M, Demirag A, et al. Giant adrenal myelolipoma associated with small bowel leiomyosarcoma: a case report. Turk J Gastroenterol 2006;17(2):126–129. PMID: 16830297.
5. Lam AK. Update on adrenal tumours in 2017 World Health Organization (WHO) of endocrine tumours. Endocr Pathol 2017;28(3):213–227. DOI: 10.1007/s12022-017-9484-5
6. Hoeffel CC, Kowalski S. Giant myelolipoma of the adrenal gland: natural history. Clin Radiol 2000;55(5):402–404. DOI: 10.1053/crad.2000.0089
7. Akamatsu H, Koseki M, Nakaba H, et al. Giant adrenal myelolipoma: report of a case. Surg Today 2004;34(3):283–285. DOI: 10.1007/s00595-003-2682-4
8. Albala DM, Chung CJ, Sueoka BL, et al. Hemorrhagic myelolipoma of adrenal gland after blunt trauma. Urology 1991;38(6):559–562. DOI: 10.1016/0090-4295(91)80180-f
9. Sanders R, Bissada N, Curry N, et al. Clinical spectrum of adrenal myelolipoma: analysis of 8 tumors in 7 patients. J Urol 1995;153(6):1791–1793. DOI: 10.1016/S0022-5347(01)67307-5
10. Nabi J, Rafiq D, Authoy FN, et al. Incidental detection of adrenal myelolipoma: a case report and review of literature. Case Rep Urol 2013;2013:789481. DOI: 10.1155/2013/789481
11. Decmann A, Perge P, Toth M, et al. Adrenal myelolipoma: a comprehensive review. Endocrine 2018;59(1):7–15. DOI: 10.1007/s12020-017-1473-4
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.